What's the difference between sadness and depression?
It’s common to go through a patch of feeling sad or blue, perhaps when the world seems a bit duller, or it gets harder to get moving. It may come in response to the dark and cold weather, it may come because of the death of a loved one, or it may come because a few things haven’t been working out for you lately. So where do we draw the line between sadness and depression? What is depression exactly? How do we diagnose it? And are there different types?
Depression is a common and at times overused word, so much so that in conversation it can mean anything from a bad mood to a chronic and debilitating condition requiring hospitalisation, and everything in between.
The difference between sadness and depression relate to:
The number of symptoms experienced,
How intense the mood is,
How long the mood lasts, and
The impact of the mood on a person’s ability to function in the various areas of their lives.
About depression and depressive disorders
It may be easier to think about depressive disorders as being a category, rather than one single thing.
One common type of depressive disorder is known as Major Depressive Disorder. This fits most people’s idea of what depression is pretty well. It’s characterised by the symptoms below [1]:
A low mood most of the day, nearly every day
Lack of interest in activities that were previously enjoyed,
Significant changes in weight or appetite,
Difficulty sleeping,
Feeling physically slow or keyed up and agitated
Loss of energy or tiredness
Feelings of worthlessness and guilt nearly every day
Difficulty thinking/making decisions/concentrating
Thoughts about suicide or dying
To fit the criteria, among other considerations a person must experience one of the first two symptoms, and have at least five of these symptoms overall, for at least two weeks. The symptoms must also interfere with a person’s functioning.
Added to a diagnosis of Major Depressive Disorder there can be a number of things called specifiers. These include (but are not limited to) things such as the addition of melancholic features, catatonia, psychotic features or seasonal patterns (in which episodes of depression occur during autumn or winter).
For example, what we may consider to be Postnatal Depression (which we blogged a bit about here) is not a separate type of depression, but instead is classified as Major Depressive Disorder with the specifier "with peripartum onset".
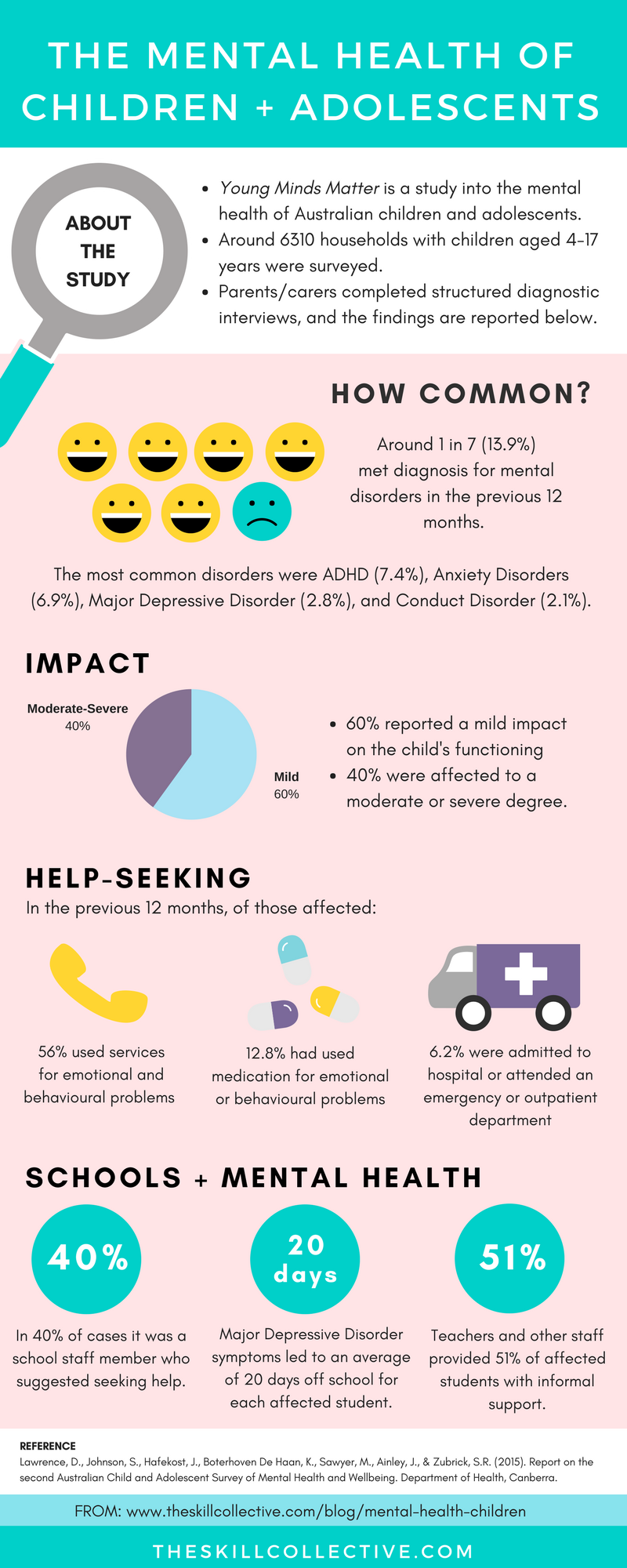
The onset of Major Depressive Disorder can happen any time in life, but peaks in the 20s, and is more common in females than males. Depression will affect about 20% of Australians sometime in their lifetime, with around 3% affected at any one point in time [2].
Although this is a common type of depression, there are other types of depression which are experienced slightly differently. Other depression diagnoses include:
Disruptive Mood Dysregulation Disorder
Premenstrual Dysphoric Disorder
Substance/medication Induced Depressive Disorder,
Depressive Disorder due to a Medical Condition,
Persistent Depressive Disorder
Other Specified Depressive Disorder, and
Unspecified Depressive Disorder
These are all wordy labels, and explanations on the meaning of each label and the difference between them are probably best left to face-to-face discussions with a mental health professional.
Dysthymia - when your depressed mood drags on...
One other type of depressive disorder that is quite common, and deserves a closer look is Persistent Depressive Disorder, also known as Dysthymia. It refers to a condition characterised by the following symptoms [1]:
Depressed mood for most of the day, more days than not for at least two years
Two or more of the following: Poor appetite or overeating, Insomnia or hypersomnia, Low energy or fatigue, Low self esteem, Poor concentration or difficulty making decisions, Feelings of hopelessness
No relief from the symptoms for more than two months at a time
Symptoms cause clinically significant distress or impairment
As with Major Depressive Disorder, there are a number of other criteria and specifiers to Persistent Depressive Disorder. This diagnosis is less common than Major Depressive Disorder, but has a longer course, with symptoms present for at least two years before a diagnosis can be made.
Is depression always just about feeling down?
When speaking to mental health professionals, you may hear these types of depression referred to as “unipolar”. This means that the mood only swings one way (low).
There is also a category of mood disorders in which mood swings both ways (low and high) and they are known as Bipolar and Related Disorders. You can read more about bipolar disorder here.
If you find that your mood is getting in the way of your daily routine, why not contact us to book an appointment?
REFERENCES
[1] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
[2] Wilhelm, K., Mitchell, P., Slade, T., Brownhill, S., & Andrews, G. (2003). Prevalence and correlates of DSM-IV major depression in an Australian national survey. Journal of Affective Disorders, 75, 155-162.






How can you counter the winter blues? Check out our tips on how to boost your wellbeing during the colder months.